In just a few weeks, I will officially be an MD. As a resident, I will provide medical care to sick patients while under the supervision of senior physicians who will help hone my skills. It will be an interesting, challenging time in my life, one that gives me a little bit of anxiety, to be honest. To be sure, I have been blessed to have had wonderful clinical training. I feel good about my clinical and interpersonal skills, and I am ready to learn and to grow—and, inevitably, to make mistakes—on my path to becoming an independent physician.
My personal feelings of readiness are ostensibly substantiated by evaluations that I have received in medical school. My diploma will represent the fact that my professors have deemed me sufficiently competent to provide clinical care to patients under the dominant paradigm of competency-based medical education (CBME). And yet, in reading my evaluations over again, these checked boxes don’t necessarily assuage my anxieties. What do my evaluations really say about me as a physician-in-training—in the deep, philosophical sense?
Physicians commonly grade clinical performance using a rubric that most outside the field are not familiar with. Rather than the conventional scale of ABCDF that often vaguely represents an assessment of overall quality, a medical school evaluation is determined by specific language describing the ability of the trainee in a given domain. For example, if a student is being evaluated on the domain of “Data Gathering” in a clinical rotation, the outstanding student “obtains a complete and accurate history in an organized fashion; seeks secondary sources of information when appropriate; and adapts to different care settings and encounters.”
The medical field’s metrics for success are not intended to represent local values. Rather, it has been an important endeavor for the profession’s educational bodies—the Accreditation Council of Graduate Medical Education (ACGME), the Liaison Committee on Medical Education (LCME), the American Association of Medical Colleges (AAMC), etc.—to standardize competencies across the continuum of medical education, from medical school, through residency, and into career life. The idea is that a trainee be universally “competent” or able, in other words, to adequately perform duties across an array of domains which organized Medicine has deemed essential for students to master.
This system of evaluation has been carefully cultivated over time to solidify Medicine’s social and professional priorities. As sociologist Paul Starr, author of The Social Transformation of American Medicine, has put it, the training of medical students has been seen as essential to the “restoration of professional control” over competing systems of care, such as empirical healing, homeopathy, and non-licensed healers. From a sociological perspective, then, the goal of organized Medicine in standardizing education has been to preserve the profession’s unique social and cultural prestige. That’s why Medicine devotes such time and effort to standardizing its system of education: to guarantee the brand, as it were, of allopathic biomedicine. This form of “objective” grading acts as a sort of rhetorical cudgel against any claims that Medicine’s trainees are inadequately prepared, and thus in need of remediation and regulation by society at large.
The sociological processes of standardization are supported by the rhetorical superstructure of science. The rubrics favored by the ACGME, AAMC, et. al. have been informed by the logics of “scientific objectivity,” as Lorraine Daston and Peter Gallison have it. In their seminal text in the history of science, Objectivity, the authors describe the titular concept and illustrate that the principle that so many of us take for granted has a past, a past within a particular epistemic, social, and cultural context. In the nineteenth century, scientists began to value depictions of natural phenomena in which the subjective presence of the perceiver was assiduously avoided, favoring—as best as possible—a “true to nature” depiction of nature. The goal was to create scientific images that purported to be not the product of a human eye, but rather unmediated photorealistic reproduction. This was precisely the era in which modern Medicine coalesced into a coherent, influential social and cultural body. The impulse to erase the human lurks in our system of grading in Medicine today, as it does in other elements of its contemporary systems of diagnosis and treatment.
“Entrustable behaviors” on my evaluations have left me somewhat cold because these concepts are divorced from the throb of the human world. By pushing “objectivity” in grading, we lose the subjective dimensions of performance and assessment.
Those willing to look carefully will recognize that concepts like entrustability, competence, and other bureaucratized buzzwords are in fact descendants of Medicine’s more humanistic past. Competence is a jargonized avatar of a priori core virtues that make a doctor good. These virtues, however, are more palpable, more human, than any abstracted, “objective” conception of professional competence. Ethicists have recognized the power of such virtues and have lauded their simple efficacy, both in the clinical space and in medical education. Indeed, in my own experience the comments from professors and preceptors, written in their own voices, have mattered much more to me than the final grade. The words of these virtuous people reflect their judgment of me and my abilities and skills, both as a professional and as a human being.
To be sure, using virtues like goodness, trustworthiness, fairness, etc. as a means to guide decision-making as physicians at the system level can be a fraught enterprise. There is conceptual slippage in what exactly we mean when we say “competent” which opens the possibility that reasonable—and unfortunately, unreasonable—people may disagree on how exactly those virtues ought to be embodied. Whenever we claim universals, we run the risk of leaving out the particular, which disproportionately impacts certain segments of the population (POCs, queer folks, disabled people, etc.) who historically have not had their experience reflected in Medicine’s virtues. This is an important topic in contemporary MedEd discourse, one that I hope to address in an upcoming companion to this piece.
And yet, as an individual at a complex moment in my professional development, I take most comfort in the virtues. For it is the human connection to my professors and my peers—our subjective, personal ties—that will nourish me when medicine challenges my confidence. It is the fact that my professors—all people I admire and respect as good people and good clinicians—feel that I am ready to meet the challenges of residency which reassures me, not any collection of metrics.
In medical education, our system of assessment and evaluation should take this experiential fact seriously. It should work to engage critically with the subtle but profound facets of our humanity as developing learners, rather than resting upon an impoverished, check-box facsimile of the virtues which guide us.
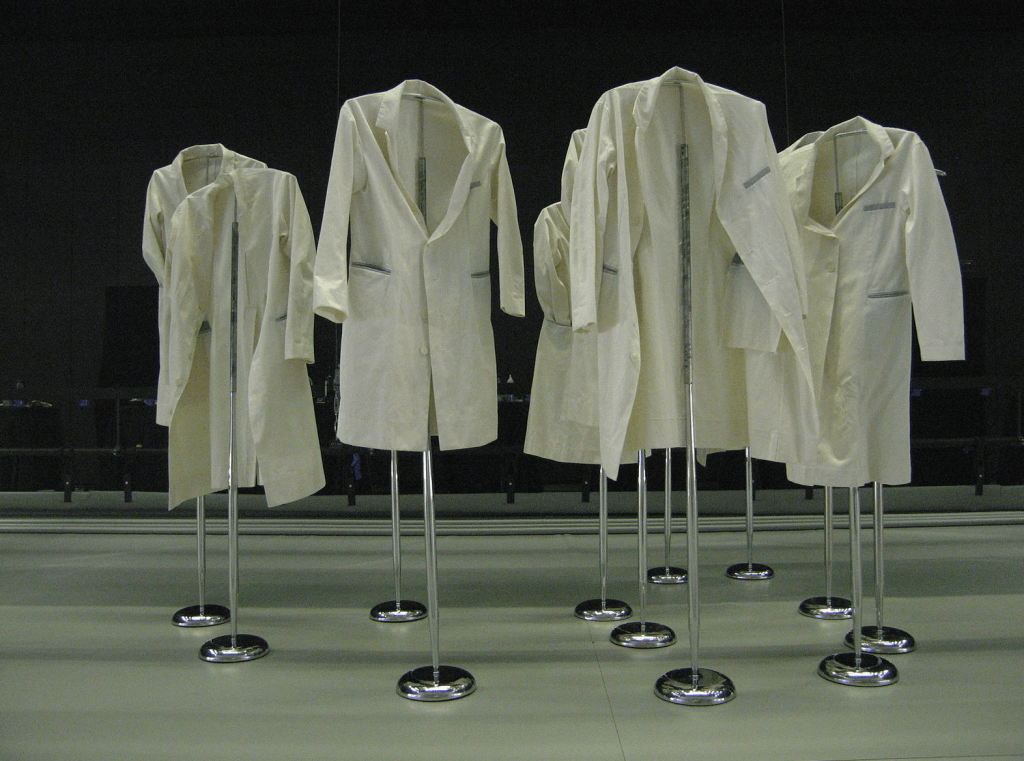
Image courtesy of Wikimedia Commons. “White coats” by Pi. Creative Commons Attribution 2.0. https://commons.wikimedia.org/wiki/File:Lab_coats.jpg