(Continue from part I: link)
In many ways, the seven years under GHQ’s occupation was transformative for the lives of Japanese people, particularly those who were sick and hospitalized. To efficiently manage limited national food resources while assuring patients’ necessary nutrient intake, in 1950, all Japanese hospitals adopted a compulsory meal supply system (kanzen kyūshoku seido, 完全給食制度). Aiming to avoid hygienic risks of self-cooking and lighten the economic burden on the inpatient’s family, all hospital meals were regulated to provide 2400 cal every day for their inpatients. No extra intake should be necessary – or would be allowed.
Created during the occupation era when food shortage was still a major concern, the compulsory hospital meal supply system prioritized sufficient nutrient intake. As food insecurity eased and economic growth accelerated from the late 1950s onward, Japanese hospitals began to pay more attention to the quality of hospital meals. One metric for evaluating the quality of hospital meals was the percentage of animal protein, which was adopted to measure the quality of hospital meals. (Nakamura, 316-7). Meanwhile, nutrition professionals appealed for further recognition of hospital meal intake as healing procedures. Such efforts to promote therapeutic diets succeeded in securing governmental acknowledgement in 1961, when the Ministry of Health, Labour, and Welfare announced a new policy of additional charge for special treatment meals (tokubetsu-shoku, 特別食). According to the new policy, hospitals could put extra charge on treatment diets for inpatients of diabetes, high blood pressure, peptic ulcer disease, and certain hepatic and renal diseases (Hara, 58). Prescribed by hospital nutritionists with consideration of patients’ conditions, these meals offered an adjusted quantity of nutrients or food texture in pursuit of patients’ quick recovery.
As part of therapeutic procedure, providing hospital meals became increasingly medical and impersonal. Even though medical effectiveness was prioritized over taste, many hospital meals became “good medicine that tastes bitter” (ryōyaku ha kuchi ni nigashi, 良薬は口に苦し). Nevertheless, patients were expected to willingly finish hospital meals for their better health, regardless of their personal dietary preference and habits. Neither seen nor heard by hospital nutritionists, patients were voicelessly labeled by their physical conditions, with their dietary lives “governed” by medical professionals. They could only use leftover food to express their feelings. According to a survey conducted at Japanese public hospitals in 1956-7, apart from sickness, the second main reason for inpatients leaving staple food was “the bad taste of side dishes” (Nihon byōin kyūshoku kenkyūkai, 207). In addition to sickness, the main causes of side dish leftovers were “bad flavor” and “dislike” of the taste (Nihon byōin kyūshoku kenkyūkai, 208).
From the late 1950s, this problem of hospital meal leftovers started to draw nutritionists’ attention. In 1960, the Japanese Hospital Meal Research Society (Nihon byōin kyūshoku kenkyūkai, 日本病院給食研究会) published a new edition of Hospital Meals: Common Menus (Byōin kyūshoku ippanshoku kondate, 病院給食一般食献立) and brought the system of “multiple menus” (Fukusū kondate, 複数献立) to the center of discussion of hospital meals. To increase patients’ appetites and reduce leftover hospital meals, some public hospitals began to offer their inpatients selectable diets. The book detailed the experiment at the National Osaka Hospital. There, inpatients that were not prescribed special treatment meals could select their lunch and dinner from two options respectively. The book went on to introduce the methods of creating the system of “multiple menus” and sample menus, hoping more Japanese hospitals would adopt this practice (Nihon byōin kyūshoku kenkyūkai, 213-5).
Designed to grant patients more control over their dietary lives, this patient-centered initiative faced much criticism at first. Opponents of this new system believed it would make patients picky eaters and hospital management more challenging (Nihon byōin kyūshoku kenkyūkai, 209). However, applauded by most patients, this system became popular from the mid-1960s onward. In addition to the popularization of selectable hospital meals, in 1973, the uniform dietary requirement of 2400 cal for regular hospital meals was replaced by guidelines on preparing hospital meals to meet personal nutritional needs of patients (Nakamura, 317).
Enjoying an increasingly diverse food culture during the period of rapid economic growth and prosperity, Japanese people developed higher expectations for hospital meals as an essential part of healthcare. By the late 1980s, in the middle of rising discussion of reframing Japan’s healthcare as “service business,” patients’ desires for gourmet foods had urged many hospitals to better the taste of their meals. Experienced nutrition professionals also studied and shared their wisdom of cooking delicious hospital meals. From 1986 to 1991, the Regional Nutritional Improvement Research Society (Chiiki eiyō kaizen kenkyūkai, 地域栄養改善研究会) published its four-volume series titled Menus of Delicious Hospital Meals (Oishii byōin kyūshoku menyū shū, おいしい病院給食メニュー集). Introducing detailed recipes and nutritional facts of over 1200 popular dishes among hospital patients nationwide, the book aimed to help more hospitals improve the quality of hospital meals.
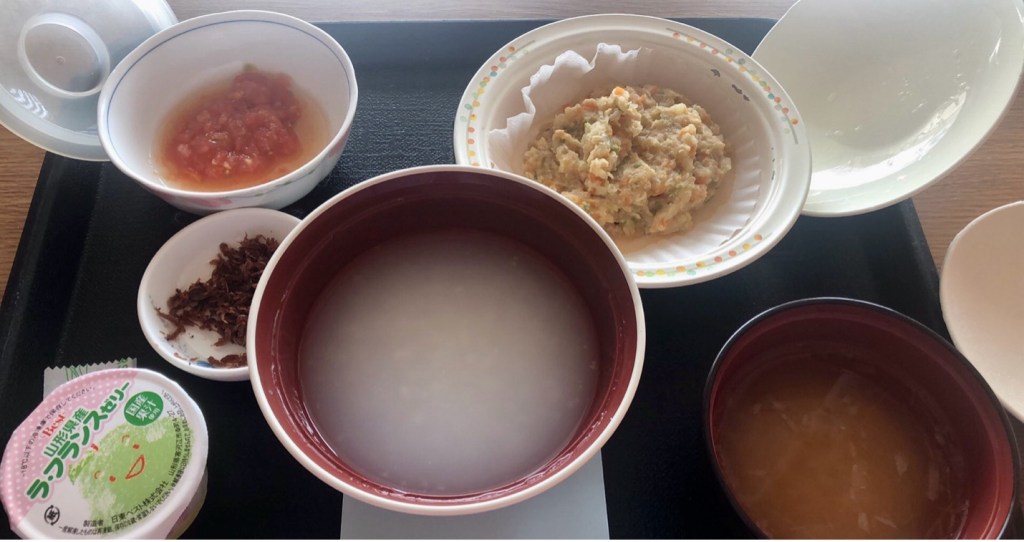
In 1995, the Annual Report on Health and Welfare (Kōsei hakusho, 厚生白書) highlighted the reconceptualization of healthcare and publicly acknowledged it as “service business” in Japan. According to the Annual Report, over 60% of surveyed Japanese citizens understood healthcare as “service business” and themselves as “customers” of hospitals. Medical professionals were expected to be not only experts but attentive carers (Ibe, 67-8). Since then, diversification of hospital meals has reflected patients’ pursuit of more individualized healthcare and better quality of life (QOL) during hospitalization. Like restaurants, hospitals began to include dishes cooked with seasonal ingredients. In response to patients’ demand, some hospitals also work closely with local farmers and cooking specialists to provide traditional cuisines. These foods, usually specially designed to resemble the homelike local cuisines, are to provide not only good taste but a sense of intimacy and emotional healing (Kimura, 30).
In postwar Japan, the transformation of hospital meals mirrored dramatic economic and social transformations as well as the reconceptualization of healthcare and patient-hospital relationship. From the 1950s onward, nutrition professionals and hospitals have gradually acknowledged the necessity of providing both healing and tasty hospital meals. From voiceless passive recipients to consumers of diversified hospital meals of better taste, Japanese patients are moving closer to the center of healthcare.
References:
Kyoko Kimura, “Dentōshoku wo byōin kyūshoku ni toriirete,” Nōchū sōken chōsa to jōhō, no. 40 (January 2014), pp. 30.
Masatoshi Hara, Kijun kyūshoku seido to sono jissai: nihon no byōin kyūshoku, Tokyo: Daiichi shuppan, 1982.
Nihon byōin kyūshoku kenkyūkai, Byōin kyūshoku ippanshoku kondate shinpen, Tokyo: Daiichi shuppan, 1960.
Teiji Nakamura, “History of Japanese nutrition therapy and response to an aging society,” Journal of Japanese Society for Parenteral and Enteral Nutrition, vol. 34, no. 5 (2019), pp. 316-9.
Toshiko Ibe, “The Late Arrival of ‘Service in Healthcare’,” Keio SFC Journal, vol. 6, no. 1 (2007), pp. 66-77.