Jennifer & April Edwell // February is American Heart Month.
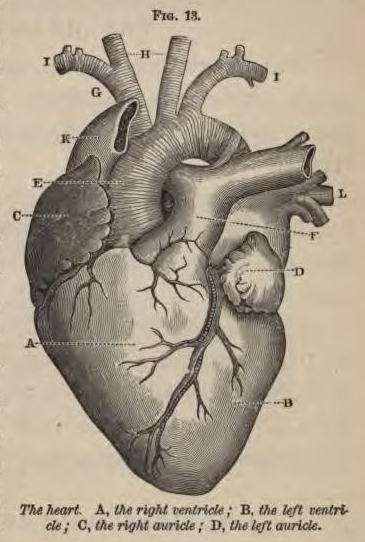
The heart is an amazing organ that deserves our fascination and veneration. There it is tirelessly beating inside your chest right now, running on its own electricity, steady and miraculous.
In adults, heart problems often arise because something that used to work has broken down [1]. The valves, like doors in old houses, get stiff and creaky. The pipes don’t flow as well and develop blockages. However, children’s hearts are a different story. Hearts can be broken from the get-go. Sometimes the blueprints are incomplete, or the construction phase gets interrupted. Hallways and large pipes end up going to the wrong rooms. The sinks all empty into the bedroom, or the bathtub doesn’t have a drain. Or someone forgot to build the living room altogether, so everyone is crowded in the kitchen. These structural problems are called congenital heart defects (CHD) [2]. Because these defects can be very serious, these hearts often require urgent renovation.
Many children born with a CHD undergo open heart surgery. Surgeons cut through the sternum and open the chest. They may put the patient on cardiopulmonary bypass, where the heart stops beating altogether and machines do the business of moving blood around and putting oxygen into it. Open heart surgery is a big deal for an adult–imagine trying to reconstruct the heart of tiny baby!
In this post, we reflect on the development of pediatric cardiology [3]. Years ago, physicians were aware that children (especially newborns) were often afflicted with “blue-disease,” or Cyanosis Neonatorum, yet medical practitioners struggled to explain—let alone treat—this fatal condition.
In 1789, Michael Underwood described several malformations of the heart in his text A Treatise on the Diseases of Children. He wrote:
“The peculiarity is sometimes in the pulmonary artery, which is constricted or closed as it rises from the right ventricle; at others, in the septum cordis, which has an unnatural opening, affording a free communication between the two ventricles; and sometimes in the imperfect closure of the foramen ovale, or the canalis arteriosus” (62) [4].
Describing these anatomical variations was a major feat. However, identifying them in a living child was nearly impossible, and treating them was out of the question. Underwood believed that medical “art has, evidently, nothing to offer” these children (63).
David Hosack (1797) references Underwood in his account of a young patient. The infant, at intervals of 10-15 minutes, “became of a dark livid blueish color” and “manifested every symptom of approaching death” (508). Hosack decided to pursue a novel course of treatment; he “applied a small blister upon the breast, and two others behind the ears; cataplasms, composed of rye meal, vinegar and mustard, to the soles of the feet; bathed its whole body with warm brandy […], and, from time to time, we attempted to give it a spoonful of wine whey” (508). As the condition of the child continued to deteriorate, Hosack administered a “stimulating bath,” where the child was submerged to its neck in warm water mixed with Peruvian bark and spirits (509). Hosak reports that the child was “uniformly relieved by the use of the bath. Since that time the child has had no return of the disease, and is at present in perfect health” (509). At the end of the article, Hosack deduces that “during the suspension of respiration, the blood ceases to circulate through the lungs, and passes by the former route through the foramen ovale” (510).
Another case is reported by John S. Dorsey in 1812. In this case, the child required recitation at birth, and then lived for several years. Dorsey writes that, by the age of two, she was “intelligent and fond of exercise” (69). However, she was “at all times blueish and livid” and experienced “frequent syncope” (69). Dorsey states that “the peculiarities of those children in whom the foramen ovale of the heart remains open, all appeared in this little girl” (69). After the child’s death, Dorsey conducted an autopsy. He describes her throat, lungs, heart. The article ends with a “mic drop.” Dorsey writes, “But the most singular circumstance was the distribution of the great arteries. The pulmonary was extremely small—the aorta of unusual size, and communicating with both ventricles” (69, emphasis in original). The reader is meant to share Dorsey’s astonishment.
Underwood’s Treatise as well as Hosack and Dorsey’s cases illustrate the difficulty of interpreting symptoms and determining effective interventions for infant patients. Nineteenth century physicians understood that “a variety of maladies […] interfere with the due aeration of the blood” (Meigs 637). Over time, physicians recognized that blue babies often have several co-occurring cardiac malformations: a hole between the lower chambers, an obstruction between the heart and lungs, a misplaced aorta, and an overly thick heart wall. These structural anomalies, described by E′tienne-Louis Arthur Fallot in 1888, are referred to as “tetralogy of Fallot” (Evans 2008).
In the 1940s, Helen Taussig (a female cardiologist), Vivien Thomas (a black surgical technician), and Alfred Blalock innovated a procedure to help blue babies: the Blalock-Thomas-Taussig Shunt (more commonly called the Blalock-Taussig or BT shunt).[5] Taussig, a pediatrician at Johns Hopkins Hospital, conceived of an intervention for tetralogy of Fallot after noticing that infants with a patent ductus arteriosus (PDA)–a connection between the aorta and pulmonary artery—didn’t turn blue like other babies (Joyner et al. 119). Taussig envisioned creating a surgical PDA to allow more blood to get to the lungs. She presented her idea to Blalock and Thomas, who had some experience creating artificial ductus systems for a different condition (Joyner et al. 120). Thomas developed the shunt procedure, and Blalock performed it on human patients. This was the first successful surgical treatment for blue babies.
Since then, our understanding of hearts—their development and their particularities—and our ability to repair them has improved significantly. There are now several medical specialties that care for children and their hearts: pediatric and congenital cardiology, cardiac surgery, and intensive care. Physicians use echocardiographic imaging to better understand the malformation. Then, surgeons work to repair the heart by doing one or more procedures, such as an arterial switch operation, Fontan procedure, the Sano Procedure, the Norwood Procedure, or Rashkind atrial septostomy. After surgery, specially trained physicians and nurses take care of these children in the ICU.
We are much better at fixing the hearts of children than we used to be. Many infants with CHDs receive life-giving repairs and go on to live ordinary lives. They play sports, participate in politics, and pursue careers. Some even become healthcare providers themselves. All without ever taking a Peruvian bark bath.
Endnotes
[1] In general, the heart has four chambers. Imagine it like a house. There are two rooms upstairs (the atria) and two rooms downstairs (the ventricles). Blood from the body enters the heart on the right side in the upper chamber. This blood is blue and depleted of oxygen. It passes through a valve into the “downstairs” ventricle—a thick chamber that forcefully pumps blood out of the right side of the heart and into the lungs. There, the blood turns from blue to red as it picks up oxygen. The newly oxygenated blood re-enters the heart in the “upstairs” left atrium before passing down into the left ventricle. Then, the blood is pumped to the body.
[2] CHDs are the most common type of birth defect.
[3] For more about the history of hearts, we recommend Sandeep Jauhar’s Heart: A History and Thomas Morris’ The Matter of the Heart: A History of the Heart in Eleven Operations.
[4] The foramen ovale is a small hole between the atria (the heart’s upstairs rooms) that typically closes shortly after birth. When the hole remains open, it is called a patent foramen ovale (PFO).
[5] This story is represented in the iconic 2004 film Something the Lord Made.
Works Cited
Dorsey, John S. “Case and Dissection of a Blue Female Child.” The New England Journal of Medicine, vol. 1, no. 1, 1812, p. 69.
Evans, William N. “‘Tetralogy of Fallot’ and E ́tienne-Louis Arthur Fallot.” Pediatric Cardiology, vol. 29, 2008, pp. 637–640. doi: 10.1007/s00246-007-9186-8
Hosack, David. “Singular Case of Disease in Infancy.” Medical Repository, vol. 1, no. 1, 1797, p. 507.
Jauhar, Sandeep. Heart : A History. Farrar, Straus and Giroux, 2018.
Joyner, Alisha, B.S., Charles J. Yeo M.D., and Maxwell, Pinckney J,I.V., M.D. “Vivien Thomas: Master Craftsman, Gifted Teacher, and Unsung Hero.” The American Surgeon, vol. 81, no. 2, 2015, pp. 118-120.
Meigs, Charles Delucena. “Chapter XXIV: Cyanosis Neonatorum.” Obstetrics: The Science and the Art, 1849, pp. 637–66.
Morris, Thomas. The Matter of the Heart : A History of the Heart in Eleven Operations. The Bodley Head, An Imprint of Vintage Publishing, 2017.
Underwood, Michael. “Imperfect Closure of the Foramen Ovale, and Canalis Arteriosus; with Other Preternatural Conformations of the Heart.” A Treatise on the Diseases of Children, 1789, pp. 62–67.